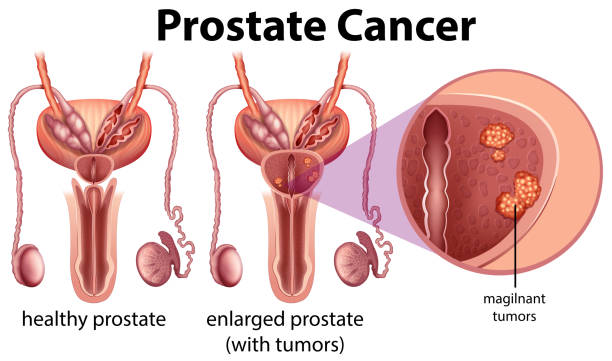
Prostate cancer is among the most common male cancers. It originates in the prostate gland, which plays a crucial role in male fertility. In India, prostate cancer is the second most frequently diagnosed cancer in men, with an incidence rate steadily increasing due to longer life expectancy and lifestyle factors. Globally, the World Health Organization reports over 1.4 million new prostate cancer cases annually, with a mortality rate nearing 375,000 deaths each year.
Dr. Manish Kumar, an eminent medical oncologist and founder, shares:
“Over the past decade, immunotherapy has created new avenues in prostate cancer care. It works not by directly killing cancer cells, but by empowering the immune system to recognize and destroy them. For select patients, it can lead to prolonged survival and an improved quality of life, especially when combined with other modalities. However, the decision to use immunotherapy must always be personalized based on cancer stage, genetic profile, and prior treatments.”
This blog aims to help you make informed decisions for yourself or your loved ones.
Curious about how the immune system can fight prostate cancer? Let’s uncover the different immunotherapy options available.
Types of Immunotherapy Used for Prostate Cancer
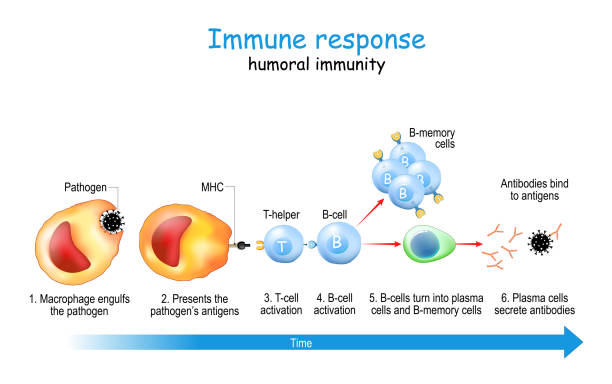
Immunotherapy uses the body’s natural defenses to fight cancer. Several types are gaining prominence based on clinical evidence.
Here’s an overview of the key types:
Sipuleucel-T (Provenge):
This is the first FDA-approved cancer vaccine specifically for advanced prostate cancer. It works by stimulating the patient’s immune cells outside the body and reintroducing them to target prostate cancer cells.
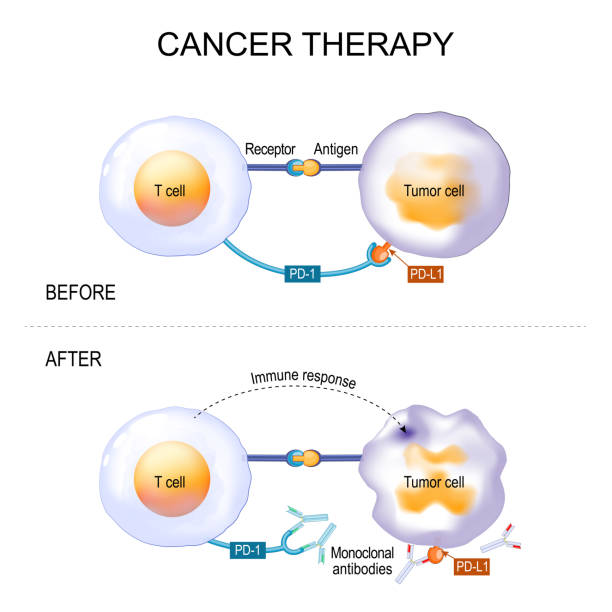
Checkpoint Inhibitors:
These include PD-1/PD-L1 and CTLA-4 inhibitors, which work by “releasing the brakes” on immune cells so they can attack cancer more effectively. While their approval is currently limited, they may be considered in tumors with high microsatellite instability (MSI-H) or mismatch repair deficiency (dMMR).
CAR T-Cell Therapy:
Although still under clinical trials for prostate cancer, this therapy involves modifying the patient’s T-cells to better recognize and destroy cancer cells.
Cytokine Therapy:
These are proteins that help regulate immune responses. Interleukins and interferons have been tested, though their role in prostate cancer is still under evaluation.
Oncolytic Virus Therapy:
This involves using genetically modified viruses to infect and kill cancer cells while also activating immune responses.
Dr. Manish Kumar, a trusted specialist in Immunotherapy Treatment for Prostate Cancer, notes:
“Sipuleucel-T has opened doors, but the future lies in combination therapies. Using immunotherapy with hormone therapy, chemotherapy, or targeted agents holds great promise. Clinical trials in India are beginning to explore this synergy.”
Not all prostate cancer patients qualify for immunotherapy. Let’s understand the eligibility.
Who Is Immunotherapy For
Determining eligibility requires a thorough clinical and genetic evaluation. Here’s who typically qualifies:
Patients with Advanced, Metastatic Cancer: Particularly those who are resistant to hormone therapy (castration-resistant prostate cancer).
Patients with dMMR or MSI-H Genetic Profiles: These genetic mutations make tumors more likely to respond to checkpoint inhibitors.
Those with Asymptomatic or Minimally Symptomatic Disease: For example, Sipuleucel-T is most effective when administered before the disease becomes too advanced or symptomatic.
Patients in Clinical Trials: Many emerging therapies are available only through trials. Participation can offer early access to innovative treatments.
Low Tumor Burden and Good Performance Status: A strong immune system is key to maximizing the effect of immunotherapy.
Starting a new treatment can feel overwhelming. Here’s a look at what immunotherapy entails.
What to Expect During Immunotherapy

Undergoing immunotherapy for prostate cancer is quite different from traditional chemotherapy or radiation. Here’s what patients can typically expect:
Treatment Schedule:
Treatments are usually given via infusion, either weekly or every few weeks, depending on the type and protocol. Sipuleucel-T, for instance, involves three infusions over about a month.
Monitoring and Imaging:
Periodic blood tests and imaging help assess the effectiveness of treatment. Unlike chemo, response to immunotherapy may take longer to appear.
Side Effects:
Most patients tolerate immunotherapy well. Common side effects include fever, chills, fatigue, joint pain, and occasionally, immune-related complications like colitis or dermatitis.
Lifestyle Impact:
Immunotherapy is generally outpatient-based and allows most patients to maintain a normal lifestyle, including work and light exercise.
Psychological Support:
Adjusting to a new form of treatment can be emotionally taxing. Many centers offer counseling and support groups.
Dr. Manish Kumar, a founder & renowned hematological oncologist, emphasizes:
“Patient education is essential. Unlike chemotherapy, immunotherapy works behind the scenes. You might not feel immediate results, but your body is gearing up for a stronger, more targeted response. Patience and consistent follow-up are vital.”
Still comparing treatment options? Let’s see how immunotherapy stacks up against traditional prostate cancer treatments.
Immunotherapy vs. Other Prostate Cancer Treatments
Understanding how immunotherapy compares to traditional prostate cancer treatments can help patients and families make informed decisions. Here’s how it stacks up against hormone therapy, chemotherapy, and radiation therapy across key factors
How Each Treatment Works
- Immunotherapy trains the immune system to detect and destroy cancer cells.
- Hormone therapy lowers testosterone to slow cancer growth.
- Chemotherapy uses drugs to kill rapidly dividing cells.
- Radiation therapy targets localized tumors with high-energy beams.
When It’s Most Effective
- Immunotherapy works best in patients with specific genetic markers or advanced, treatment-resistant cancer.
- Hormone therapy is effective in early or metastatic stages.
- Chemotherapy is used for advanced or aggressive cases.
- Radiation therapy is suitable for localized tumors.
Side Effects to Consider
- Immunotherapy: Usually mild—fatigue, skin rash, or fever.
- Hormone therapy: Hot flashes, bone thinning, mood changes.
- Chemotherapy: Nausea, fatigue, hair loss, low immunity.
- Radiation therapy: Fatigue, urinary or bowel discomfort.
Long-Term Impact
- Immunotherapy: May improve survival in select patients.
- Hormone therapy: Resistance may develop over time.
- Chemotherapy: Risk of long-term toxicity.
- Radiation therapy: Possible recurrence in some cases.
Use in Combination
- Immunotherapy shows high potential in combined approaches.
- Hormone therapy is often paired with radiation or chemo.
- Chemotherapy is commonly combined for advanced cases.
- Radiation therapy is sometimes used with hormone therapy.
While traditional treatments remain essential, immunotherapy offers a growing, personalized option—especially in cases where standard approaches fall short. Its integration into multi-modal treatment plans reflects the future of precision cancer care.
Still have questions? Let’s answer the most common ones about prostate cancer immunotherapy.
FAQ
1. Is immunotherapy approved for all prostate cancer patients?
No, immunotherapy is approved only for specific cases, such as those with advanced, castration-resistant prostate cancer or tumors with certain genetic markers like MSI-H or dMMR.
2. What are the side effects of prostate cancer immunotherapy?
Most patients experience mild flu-like symptoms. Rarely, immune-related side effects like inflammation of the colon, liver, or lungs may occur, which are usually manageable with corticosteroids.
3. Can immunotherapy cure prostate cancer?
Immunotherapy is not a cure but can offer extended survival and better quality of life. It’s most effective when integrated early in resistant cases.
4. How long does immunotherapy treatment last?
The duration varies. Sipuleucel-T is typically completed in about a month, while checkpoint inhibitors may be given for several months depending on response.
5. How successful is Sipuleucel-T in prostate cancer?
Studies show that Sipuleucel-T extends survival by an average of 4.1 months. Its success is most evident when used early in asymptomatic, metastatic cases.
6. Is genetic testing required before immunotherapy?
Yes, especially when considering checkpoint inhibitors. Testing for MSI-H, dMMR, or BRCA mutations helps identify if the patient is likely to benefit.